Energy Prices and Poverty: A Growing Crisis for the Vulnerable
Energy prices have exacerbated poverty and inequality, particularly affecting those who are already vulnerable, among the most impacted are disabled individuals and people with chronic illnesses, who often face higher energy consumption due to their unique needs. This situation underscores the urgent necessity for targeted support and policy interventions to prevent these populations from slipping further into energy poverty.
Energy poverty has far-reaching consequences that extend into the realm of child poverty, creating a devastating cycle. When families cannot afford their energy bills, they often face the harsh reality of having to choose between heating their homes and buying food. This dire situation leaves children cold and hungry, undermining their health, well-being, and ability to thrive. Exposure to cold environments can lead to respiratory issues and other health problems, while inadequate nutrition hampers growth and cognitive development. The stress and instability caused by energy poverty can also affect children’s emotional and psychological health, perpetuating a cycle of poverty that is difficult to break.
The Disproportionate Impact on Disabled and Chronically Ill Individuals
Disabled individuals and those with chronic illnesses often rely heavily on energy-intensive medical equipment and environmental controls to maintain their health and well-being. For instance, they may require:
- Medical Devices: Ventilators, oxygen concentrators, and dialysis machines, which are vital for survival but consume significant amounts of electricity.
- Heating and Cooling: To manage symptoms exacerbated by temperature extremes, these individuals may need to keep their homes warmer in winter and cooler in summer.
- Mobility Aids: Electric wheelchairs and mobility scooters need regular charging.
- Extended Home Stays: Many disabled individuals spend more time at home, increasing their overall energy consumption for lighting, cooking, and other daily activities.
Mental Health and Energy Poverty: A Vicious Cycle
The intersection of mental health and energy poverty represents a critical yet often overlooked aspect of the broader poverty landscape. Individuals struggling with mental health disorders frequently face unique challenges that lead to increased energy consumption, exacerbating their financial burdens. Understanding this connection is vital to developing effective interventions and support mechanisms.
The Impact of Mental Health on Energy Consumption
Mental health disorders can significantly influence daily living patterns and energy usage. For example, individuals with Obsessive-Compulsive Disorder (OCD) may engage in repetitive behaviors that increase their energy consumption. A person with OCD might repeatedly wash their hands, clean their living spaces, or check locks and appliances, all of which contribute to higher utility bills. Similarly, other mental health conditions can lead to behaviors and needs that drive up energy use:
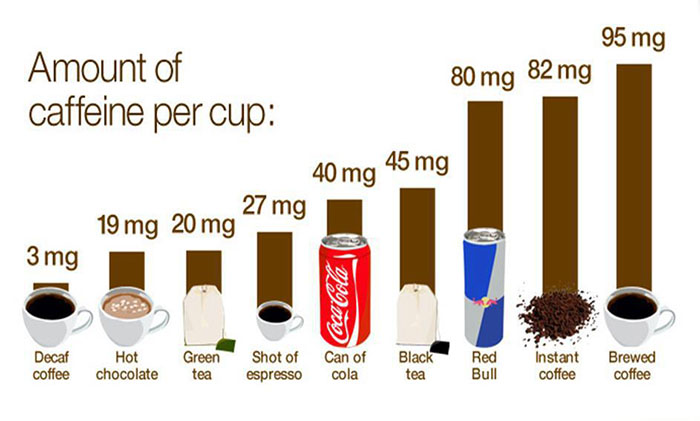
- Anxiety and Depression: Individuals may spend more time at home, leading to increased use of lighting, heating, or cooling. They might also leave lights and electronics on as a comfort mechanism or due to a lack of motivation to turn them off.
- Insomnia: Those who struggle with sleep disorders may stay up late or wake up frequently during the night, using more energy for lighting, heating, or entertainment like TV and computers.
- Bipolar Disorder: During manic phases, individuals may engage in more activities that consume energy, such as excessive cleaning, cooking, or running electrical appliances.
- Post-Traumatic Stress Disorder (PTSD): People with PTSD might need to maintain certain environmental conditions, like keeping lights on at night, to feel safe, thus increasing their energy use.
These behaviors are often necessary for managing symptoms and maintaining a sense of control and comfort, but they also result in higher energy costs.
Example: OCD and Increased Energy Use
Consider Sarah, who lives with OCD. Her condition compels her to frequently wash her hands, and clean her home. This means her water heater, washing machine, and vacuum cleaner are used far more than in an average household. Additionally, she often leaves lights on throughout the house to reduce anxiety about intruders or accidents. These necessary actions for managing her mental health lead to significantly higher energy bills, pushing her closer to energy poverty.
Addressing the Issue
To support individuals with mental health disorders and mitigate the risk of energy poverty, several strategies can be implemented:
- Specialized Tariffs: Energy providers should offer tariffs that cater to the specific needs of individuals with mental health conditions, similar to those proposed for disabled individuals.
- Financial Assistance: Enhanced subsidies or grants can help cover the increased costs associated with higher energy consumption.
- Energy Efficiency Programs: Providing resources and support for energy-efficient appliances and home modifications can help reduce overall consumption without compromising the individual’s comfort and safety.
- Mental Health Support Services: Integrating energy management into mental health care plans can help individuals find balance and identify ways to reduce unnecessary energy use without exacerbating their conditions.
Energy poverty and mental health are deeply interconnected, creating a cycle that can be challenging to break.
Recognizing and addressing the unique energy needs of individuals with mental health disorders is crucial for developing comprehensive solutions that ensure no one has to choose between managing their mental health and affording their energy bills. By fostering a more inclusive approach, society can better support these vulnerable populations, promoting both mental and financial well-being.
Despite these increased needs, current energy tariffs do not reflect the additional costs incurred by disabled households. This has led to calls for energy providers to introduce specialized tariffs that consider the higher energy usage of disabled people, ensuring they are not disproportionately penalized by rising energy prices.
The Role of the Fuel Bank Foundation
Amidst this crisis, the Fuel Bank Foundation has emerged as a crucial lifeline for those struggling with energy costs. This charity provides emergency financial assistance to families and individuals who are unable to afford their energy bills, preventing them from having to make impossible choices between heating their homes and other essential needs. The foundation’s support extends beyond immediate financial relief, offering guidance and advocacy to help people manage their energy usage more effectively and access additional resources.
The Limitations of Current Complaints Processes
When facing unjust energy bills or service issues, consumers can lodge complaints with Ofgem, the UK’s energy regulator. However, many find this process to be unsatisfactory. Often, the resolution provided by Ofgem, if any, may only include a modest financial compensation, typically capped at £200, along with an apology from the energy provider. This outcome does little to address the ongoing financial strain faced by disabled individuals, who continue to struggle with high energy costs without meaningful relief.
Advocacy for Policy Change
There is a pressing need for the government to recognize and address the unique energy challenges faced by disabled people and disabled entrepreneurs. Given their higher energy consumption, policy measures should include:
- Specialized Tariffs: Introduction of energy tariffs that account for higher usage by disabled households.
- Increased Financial Support: Enhanced subsidies and grants to help cover the cost of essential energy consumption.
- Regulatory Reforms: Strengthening Ofgem’s mandate to ensure fairer outcomes for vulnerable consumers and more substantial penalties for energy providers who fail to meet their needs.
The government must take proactive steps to ensure that the energy market operates fairly for all citizens, particularly those who are most vulnerable. By acknowledging the specific needs of disabled individuals and implementing targeted support measures, we can work towards a more equitable and just energy system. The Fuel Bank Foundation’s efforts highlight the critical role of charity in bridging the gap, but sustainable, systemic change is essential for long-term solutions.
In conclusion, it is imperative that we prioritize the needs of those most affected, through collaborative efforts between charities, regulators, and policymakers, we can mitigate the impact of energy poverty and ensure that every household can afford to stay warm and healthy.
Citation: Mum’s cost of living warning as energy meter poverty hits record high (msn.com)