Transitioning from Working Tax Credits to Universal Credit: Implications for Self-Employed Individuals Over 60 in the UK
For self-employed individuals in the UK who are currently receiving Working Tax Credits (WTC), the transition to Universal Credit (UC) can bring significant changes. Universal Credit, which replaces six legacy benefits including WTC, has different rules and requirements that can affect how self-employed individuals manage their business and personal circumstances.
Universal Credit and Self-Employment: Key Changes
Universal Credit introduces the Minimum Income Floor (MIF), which is a major shift from the legacy benefits system. The MIF assumes that self-employed claimants earn a certain amount each month, typically equivalent to the National Minimum Wage for their expected hours of work. For those over 60, this can pose unique challenges.
- Minimum Income Floor (MIF):
- The MIF is designed to ensure that self-employed individuals are earning at least the equivalent of what they would receive if they were working full-time at the National Minimum Wage. If your actual earnings are below this level, UC will not make up the difference.
- For example, if the MIF is set at 35 hours per week at the National Minimum Wage for under 60’s, and your actual earnings fall short of this, UC will still calculate your entitlement as if you were earning this amount.
- Exceptions and Adjustments:
- There are exceptions to the MIF, particularly during the start-up period for new businesses, which lasts up to 12 months. During this period, the MIF does not apply, giving new entrepreneurs time to establish their business.
- However, for established businesses or individuals transitioning from WTC to UC, the MIF is applied immediately unless other circumstances merit an exemption.
Impact on Part-Time Self-Employed
If you are self-employed, and working part-time, you may face several challenges under UC:
- Pressure to Increase Earnings:
- UC regulations might pressure you to increase your hours or earnings to meet the MIF. If you are unable to do so, you could see a reduction in your UC payments.
- This pressure can be particularly challenging if you have limited ability to expand your business, due to market conditions, health, or other personal constraints.
- Inability to Increase Business:
- If you cannot secure more business or increase your earnings due to market saturation, competition, or lack of demand, you might struggle to meet the MIF.
- In such cases, you could be required to look for additional or alternative work to supplement your income, even if it means taking up employment outside your self-employment activities.
- Additional Responsibilities:
- If you are also a carer or a part-time student, the expectation to increase your self-employment income can become even more burdensome.
- Carers often have limited time and flexibility due to their caregiving responsibilities. Similarly, part-time students may have restricted availability due to their academic commitments.
- UC takes these factors into account, and you may be eligible for reduced work requirements. However, navigating these adjustments can be complex and requires clear communication with the Department for Work and Pensions (DWP).
Navigating the Transition
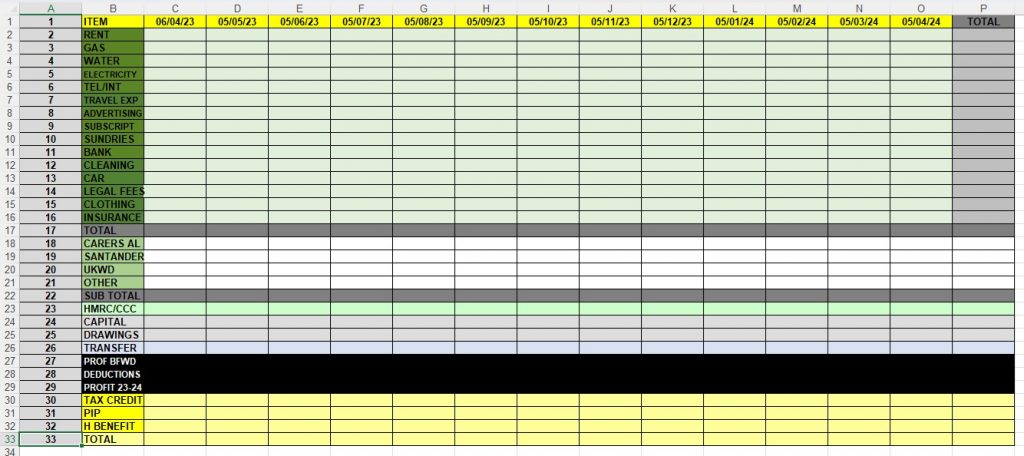
- Documentation and Reporting:
- Accurate and timely reporting of your income and expenses is crucial. Keep detailed records to ensure your UC claim reflects your actual earnings and circumstances.
- Regular updates to the DWP about changes in your work status, health, caregiving responsibilities, or educational commitments are necessary to adjust your work requirements appropriately.
- Seeking Support:
- Utilize resources available through business support organizations, such as advice on growing your business or managing finances.
- Charitable organizations and local councils may offer additional support or guidance, particularly for those with caregiving responsibilities or health issues.
- Understanding Your Rights:
- Familiarize yourself with UC regulations and your rights. The DWP website and various advocacy groups provide information that can help you understand and navigate the system.
Eligibility For Carers Allowance:
The type of care you provide
You need to spend at least 35 hours a week caring for someone.
This can include:
- helping with washing and cooking
- taking the person you care for to a doctor’s appointment
- helping with household tasks, like managing bills and shopping
Your eligibility
All of the following must apply:
- you’re 16 or over
- you spend at least 35 hours a week caring for someone
- you’ve been in England, Scotland or Wales for at least 2 of the last 3 years (this does not apply if you’re a refugee or have humanitarian protection status)
- you normally live in England, Scotland or Wales, or you live abroad as a member of the armed forces (you might still be eligible if you’re moving to or already living in an EEA country or Switzerland)
- you’re not in full-time education
- you’re not studying for 21 hours a week or more
- you’re not subject to immigration control
- your earnings are £151 or less a week after tax, National Insurance and expenses
If you are claiming Carer’s Allowance, the earnings limit and the rules around it interact with Universal Credit in specific ways. Let’s delve deeper into how these rules intersect and what it means for self-employed individuals over 60 who are also claiming Carer’s Allowance and transitioning to Universal Credit.
Understanding the Interaction Between Carer’s Allowance and Universal Credit
Carer’s Allowance Earnings Limit
Carer’s Allowance has an earnings limit, which means you cannot earn more than £151 per week (as of 2023) from employment or self-employment. If your earnings exceed this limit, you will not be eligible for Carer’s Allowance.
Universal Credit and Carer’s Element
Universal Credit provides a carer’s element if you are providing care for at least 35 hours a week for a severely disabled person. This can be claimed even if you are not receiving Carer’s Allowance, provided you meet the criteria.
Implications for Self-Employed Individuals Over 60
Minimum Income Floor (MIF) and Carer’s Allowance
- Earnings Restriction:
- Since you cannot earn more than £151 per week to qualify for Carer’s Allowance, this creates a clear boundary for your earnings. If you are self-employed, you need to manage your income carefully to stay within this limit while receiving Carer’s Allowance.
- Universal Credit Requirements:
- The Universal Credit system takes into account your role as a carer. This can reduce or eliminate the requirement to increase your hours or earnings to meet the Minimum Income Floor (MIF).
- If you are a carer and also a part-time student or have other commitments, these factors will be considered when determining your work-related requirements under UC.
Work-Related Requirements Under Universal Credit
- No Work-Related Requirements:
- If you are providing care for at least 35 hours a week, you may be placed in the “no work-related requirements” group. This means you will not be required to look for or undertake additional work to increase your income.
- Limited Capability for Work:
- If you have health issues or disabilities, you might be assessed for limited capability for work. If accepted, this could further reduce or eliminate work-related requirements.
Managing Your Income and Reporting
- Self-Employment Income Reporting:
- As a self-employed individual, you need to report your earnings and expenses accurately and regularly to both Universal Credit and Carer’s Allowance.
- Keeping detailed financial records is crucial to ensure compliance and avoid overpayment issues.
- Adjustments and Reviews:
- Regular reviews of your circumstances by the Department for Work and Pensions (DWP) will help ensure that your Universal Credit claim reflects your actual situation, including your caregiving duties and any part-time education commitments.
Practical Steps for Navigating the Transition
- Seek Advice and Support:
- Contact the DWP or seek advice from organizations like Citizens Advice to understand how best to manage your Universal Credit claim alongside Carer’s Allowance.
- Professional advice can help you navigate the rules and maximize your benefits while staying within the earnings limits.
- Understand Your Rights:
- Be aware of your rights regarding work requirements under Universal Credit. If you believe your responsibilities as a carer are not being appropriately considered, you can request a review or seek advocacy support.
- Plan Your Finances:
- Plan your self-employment activities to ensure that your earnings stay within the Carer’s Allowance threshold. This might involve adjusting your business activities or managing your workload to balance your earnings and caregiving responsibilities.
Transitioning from Working Tax Credits to Universal Credit involves understanding new rules and how they interact with existing benefits like Carer’s Allowance. For self-employed individuals over 60 who are also carers, the key is to manage your earnings to stay within the Carer’s Allowance limit while navigating the work-related requirements of Universal Credit. With careful planning, accurate reporting, and support from relevant organizations, you can effectively manage this transition and ensure your financial stability.
Navigating Universal Credit for Over 60 Self-Employed Disabled Entrepreneurs with Caring and Education Responsibilities
For a claimant over 60 who is a disabled entrepreneur working part-time for 16 hours a week, caring for someone for 35 hours a week, and studying part-time for 16 hours a week, Universal Credit (UC) will take into account several factors to determine the impact on their benefits. Let’s break down each aspect and how it will affect their UC claim.
Factors Affecting Universal Credit
- Self-Employment:
- Minimum Income Floor (MIF): The MIF may not apply if the claimant is in a category exempt from it, such as having a limited capability for work due to a disability. If the MIF applies, it assumes the claimant earns at least the equivalent of the National Minimum Wage for a set number of hours.
- Earnings Reporting: The claimant needs to report their self-employment income accurately. If the actual earnings are below the MIF, UC will calculate entitlement based on the MIF unless an exemption applies.
- Caring Responsibilities:
- Carer’s Allowance: If the claimant is providing care for at least 35 hours a week, they may be eligible for Carer’s Allowance, which has an earnings limit of £151 per week.
- Carer’s Element in UC: UC can include a carer’s element if the claimant is caring for a severely disabled person for at least 35 hours a week, even if they do not claim Carer’s Allowance. This could reduce the work-related requirements.
- Part-Time Higher Education:
- Education Commitments: Being a part-time student studying 16 hours a week will be considered in the UC work capability assessment. The claimant needs to provide details of their study schedule.
- Limited Capability for Work:
- Health Assessments: Given the claimant’s disability, they may be assessed for limited capability for work. If found to have limited capability for work or work-related activity, this will affect their UC requirements and potentially exempt them from the MIF.
Work-Related Requirements
Given the claimant’s unique circumstances, they are likely to be placed in a group with reduced or no work-related requirements. Here’s how each factor contributes to this assessment:
- Disability:
- If the claimant is deemed to have limited capability for work or work-related activity, they may not be subject to the MIF and will have fewer work-related requirements.
- Caring Responsibilities:
- Caring for someone for 35 hours a week could place the claimant in the “no work-related requirements” group.
- Part-Time Work and Study:
- While part-time work and study hours are substantial, they will be secondary considerations to the disability and caring responsibilities.
Financial Impact
- Universal Credit Amount:
- The claimant’s UC amount will be calculated based on their income from self-employment, adjusted for any MIF exemptions due to their disability.
- The carer’s element will be added if they are caring for someone for 35 hours a week.
- The claimant’s earnings from part-time work and any student income will be considered in the UC calculation, but the primary factors will be disability and caring responsibilities.
- Potential Additional Support:
- The claimant may also qualify for other forms of support, such as Disabled Students’ Allowances (DSAs) if their studies are affected by their disability.
Practical Steps for the Claimant
- Report All Circumstances:
- The claimant must provide detailed information about their self-employment income, caregiving hours, and educational commitments to the DWP.
- Seek Advice:
- Consulting with Citizens Advice or a welfare rights advisor can provide personalized guidance and ensure all benefits and exemptions are appropriately applied.
- Keep Accurate Records:
- Maintaining accurate records of income, caregiving activities, and study hours will help in managing their UC claim and any potential reviews or assessments.
For a disabled entrepreneur over 60 who is working part-time, caring for a person 35 hours a week, and studying part-time, Universal Credit will be calculated with significant considerations of their disability and caregiving responsibilities. These factors are likely to reduce or eliminate work-related requirements, and additional elements such as the carer’s element will be included in their UC calculation. Accurate reporting and seeking professional advice will help manage the complexities of their UC claim effectively.
How to Apply for Limited Capability for Work and Work-Related Activity (LCWRA)
Applying for the Limited Capability for Work and Work-Related Activity (LCWRA) component within Universal Credit involves several steps. This process is designed to assess whether your health condition or disability limits your ability to work and undertake work-related activities. Here’s a detailed guide on how to apply:
Step-by-Step Guide
- Inform the Department for Work and Pensions (DWP):
- Initial Declaration: When you apply for Universal Credit, you need to declare any health condition or disability that affects your ability to work. This can be done through your online Universal Credit account or by informing your work coach during your initial assessment meeting.
- Provide Medical Evidence:
- Fit Note: Obtain a fit note (formerly known as a sick note) from your GP or healthcare provider. This document should detail your medical condition and how it affects your ability to work. Submit this fit note to the DWP as soon as possible.
- Complete the Capability for Work Questionnaire (UC50):
- UC50 Form: The DWP will send you a UC50 form, which is a detailed questionnaire about your health condition and how it impacts your daily life and ability to work. Fill out this form accurately and thoroughly, providing as much information as possible about your condition.
- Supporting Documents: Include any additional medical evidence, such as letters from specialists, test results, or treatment plans, that support your claim.
- Work Capability Assessment:
- Assessment Appointment: You will likely be asked to attend a Work Capability Assessment (WCA), which is conducted by a healthcare professional appointed by the DWP. This assessment can take place either in person, over the phone, or via video call.
- Assessment Content: During the assessment, you will be asked questions about your health condition, daily activities, and how your condition affects your ability to perform work-related tasks. Be honest and detailed in your responses.
- Decision on Capability:
- DWP Decision: After the assessment, the healthcare professional will send their report to the DWP, who will make a decision on your capability for work and work-related activity. If they determine that you have limited capability for work and work-related activity (LCWRA), you will be placed in the LCWRA group.
- Notification:
- Outcome Letter: You will receive a decision letter from the DWP informing you of the outcome of your assessment. If you are placed in the LCWRA group, you will not be required to look for work or undertake work-related activities, and you will receive additional financial support through your Universal Credit payment.
Additional Tips
- Prepare Thoroughly: Gather all relevant medical documentation and evidence before completing the UC50 form and attending the assessment.
- Seek Support: Consider getting help from a welfare advisor or a support organization, such as Citizens Advice, to ensure your application is as strong as possible.
- Keep Records: Maintain copies of all documents and correspondence with the DWP, including fit notes, the UC50 form, and any additional medical evidence.
By following these steps and providing comprehensive evidence of your health condition, you can effectively apply for the LCWRA component of Universal Credit, ensuring you receive the support you need while managing your condition.
NON Arrival Of Migration Letters
Universal Credit migration is not done automatically, largely because the process requires individualized assessment and communication to ensure each claimant’s specific circumstances are properly addressed. This complexity necessitates a manual approach to ensure accurate and fair transitions from legacy benefits to Universal Credit.
Some critics argue that the lack of automatic migration and the delay in sending out migration letters could be a tactic to save public money. By potentially causing people to miss deadlines for transitioning to Universal Credit, the government may reduce the overall number of claimants, thereby decreasing expenditure on benefits. This suspicion highlights the need for claimants to stay proactive and informed about their transition status to avoid any unintended loss of benefits.
If the Department for Work and Pensions (DWP) already possesses all the necessary data from legacy benefits, requesting claimants to reconfirm the same information is time-consuming, not proactive, and unnecessary. This redundant process places an additional burden on claimants, many of whom may already be facing challenging circumstances. Instead of streamlining the transition to Universal Credit, it complicates the process, potentially leading to delays and errors. A more efficient approach would be to utilize existing data to facilitate a smoother, more seamless migration, thereby reducing stress on claimants and improving the overall efficiency of the system.
If you have not received a transition letter and have been informed that you are no longer eligible for Universal Credit, you have the right to take action. You can contact the Equality and Human Rights Commission (EHRC) and file a formal complaint. The Department for Work and Pensions (DWP) is currently under investigation for potentially breaching EHRC laws, and your case could contribute to this broader investigation. The EHRC is responsible for enforcing equality and human rights laws in the UK, and they can provide guidance and support in addressing any potential discrimination or mishandling of your benefits transition. Taking this step ensures your rights are protected and that any unfair treatment is formally challenged.
Conclusion
The transition from Working Tax Credits to Universal Credit in the UK brings new challenges for self-employed individuals. The introduction of the Minimum Income Floor can create pressure to increase earnings, which may be difficult due to market conditions, caregiving responsibilities, or part-time education. Understanding the new rules, keeping detailed records, and seeking support are essential steps to ensure that you can effectively manage your UC claim and continue to meet your financial needs.
For individuals under 60 looking to avoid Universal Credit sanctions related to job searching, it may be feasible to consider starting a course in higher education or launching a business. Both options can help meet UC requirements while potentially advancing your career or business prospects. Additionally, if you know someone elderly or disabled who needs support, applying for Carer’s Allowance can provide financial assistance and reduce work search requirements. If you are disabled and working part-time, you may be eligible for benefits such as the Disability Living Allowance (DLA) or Personal Independence Payment (PIP) to help with the extra costs of living with a disability. Furthermore, applying for the Limited Capability for Work and Work-Related Activity (LCWRA) component within Universal Credit can offer additional financial support and exemption from further work-related requirements if your condition prevents you from increasing your working hours.
Further Reading:
- Transitional protection if you receive a Migration Notice letter – GOV.UK (www.gov.uk)
- DWP halts benefits of 184,000 people in ‘unacceptable’ move (msn.com)
- DWP update on Universal Credit migration and adds ‘existing benefits will end’ (msn.com)
- Carer’s Allowance: Eligibility – GOV.UK (www.gov.uk)
- Who goes into the Limited Capability for Work-Related Activity (LCWRA) group and how? (benefitsandwork.co.uk)
- Work Capability Assessment – Limited Capability for Work Related Activity | Turn2us
- DWP under fire after billions in benefits go unpaid and callers suffer long waits (msn.com)
- DWP under investigation over disability benefit assessments after claimant deaths | The Independent
- Department for Work and Pensions under investigation for treatment of disabled benefits claimants | EHRC (equalityhumanrights.com)
- Contact us | EHRC (equalityhumanrights.com)