Category: Multiple Sclerosis (Page 1 of 4)

Visit Us Today!
🎉 Exciting Announcement: DisabilityUK.co.uk Launch 🎉
We are thrilled to announce the launch of our new website, www.disabilityuk.co.uk Initially planned as a rebrand of www.disabledentrepreneur.uk earlier this year, we’ve made the decision to keep both sites … Continue Reading...
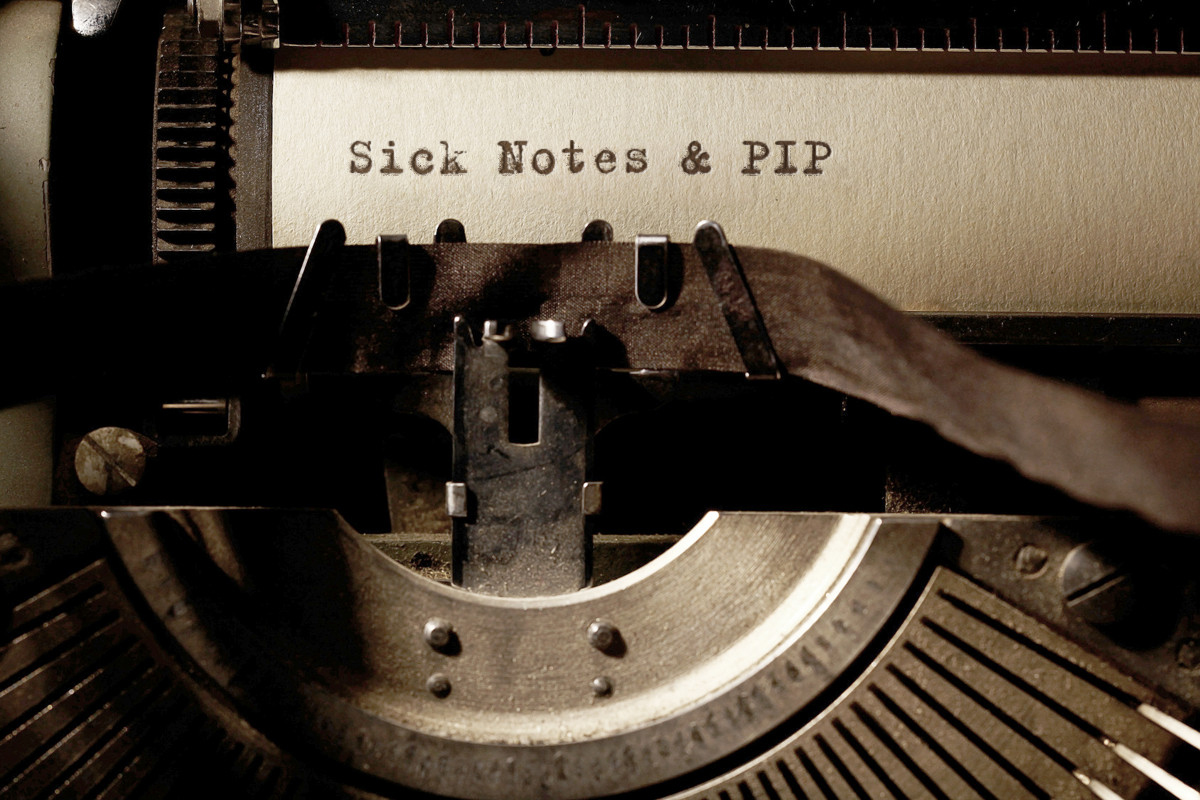
Navigating the Process: Proving Invisible Disabilities for PIP Eligibility
Invisible disabilities present unique challenges, particularly when it comes to proving eligibility for benefits like the Personal Independence Payment (PIP). While these conditions may not be immediately apparent to others, their … Continue Reading...
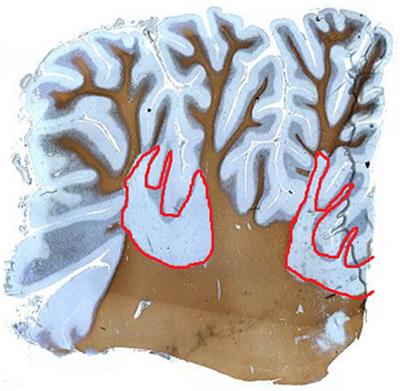
Unveiling the Startling Origins of Multiple Sclerosis: A Genetic Journey Across Millennia
Multiple Sclerosis (MS), a chronic and often disabling neurodegenerative disease, has long puzzled scientists and researchers seeking to understand its origins. In a groundbreaking study, scientists … Continue Reading...
Multiple Sclerosis FAQ
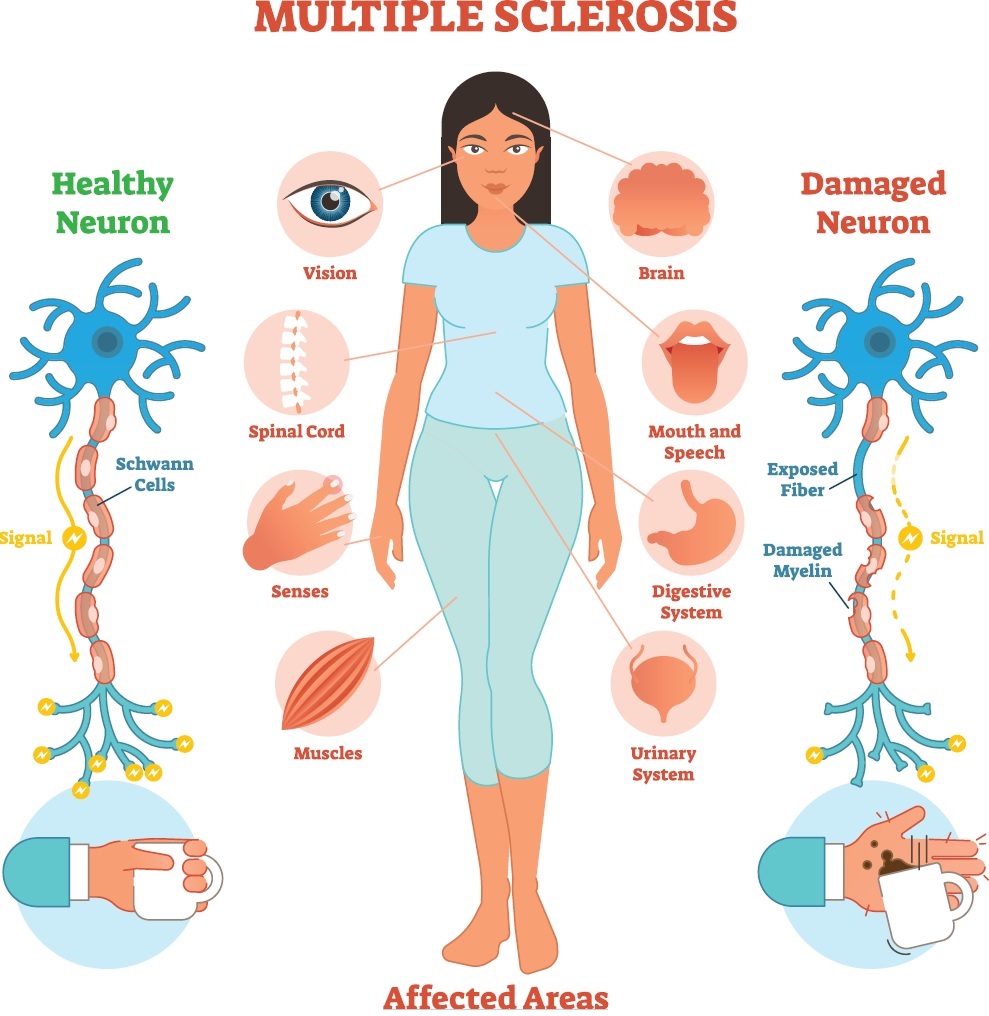
- What is Multiple Sclerosis (MS): MS is a chronic, autoimmune disease that affects the central nervous system (CNS), including the brain and spinal cord. It occurs when the immune system mistakenly attacks the protective

The Struggle for Support: Cardiff NHS and the Neglected Calls for Multiple Sclerosis Patients
Living with Multiple Sclerosis (MS) is challenging enough without having to navigate a healthcare system that seems unresponsive and neglectful. Unfortunately, this appears to be the … Continue Reading...
Embracing Life’s Uncharted Path: A Young Warrior’s Journey with Multiple Sclerosis
Today, we embark on a poignant journey into the life of a remarkable young individual, whose path is illuminated not just by the exuberance of youth but also by … Continue Reading...
Leg Numbness: Unraveling the Mystery and its Connection to Multiple Sclerosis
Leg numbness is a sensation that many people have experienced at some point in their lives. It can be a temporary inconvenience, often attributed to sitting in … Continue Reading...

Disability Discrimination.
Unmasking the Veil of Disability Discrimination: A Call for Inclusivity
Discrimination is a persistent and deeply ingrained issue in societies across the world. Among the various forms of discrimination, disability discrimination remains a grave concern. Despite significant advancements … Continue Reading...